Sterilizing Medical Devices Requires Friendly Agents
The best sterilization process for a medical device depends on the materials and methods used to assemble it

NO2 is incompatible with cellulose materials, such as paper and cardboard. It will also change the chemical structure of polyurethane, nylon and polyoxymethylene. Photo courtesy Noxilizer Inc.

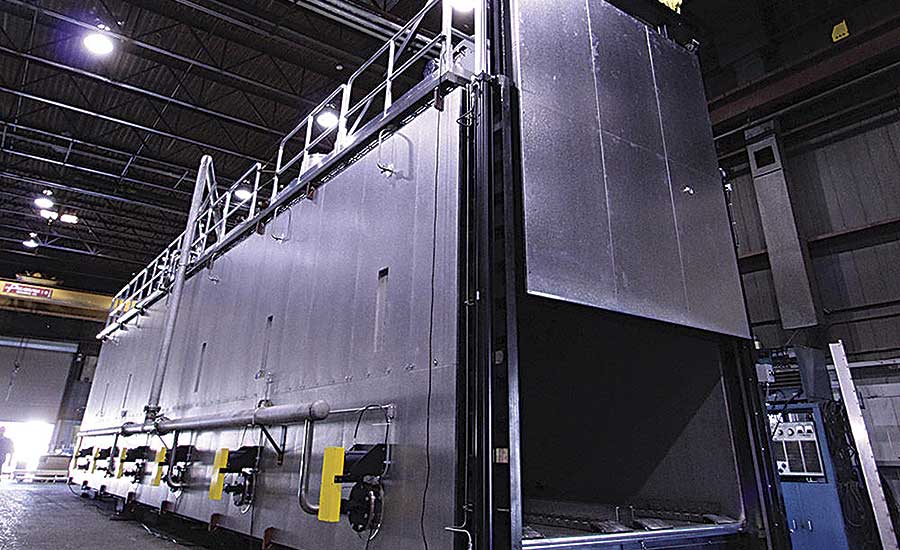
The sterilization with EO takes place in a sealed chamber. The three-phase process involves preconditioning the load, sterilization with EO, and aeration to purge the toxic gas. Photo courtesy Cosmed Group Inc.

The most common source of radiation for sterilization is cobalt-60. Rods of cobalt-60 are stacked in a column that is encapsulated by two separate layers of stainless steel. Each “pencil” of cobalt-60 is approximately 18 inches long and 0.375 inch in diameter. Photo courtesy STERIS Applied Sterilization Technologies

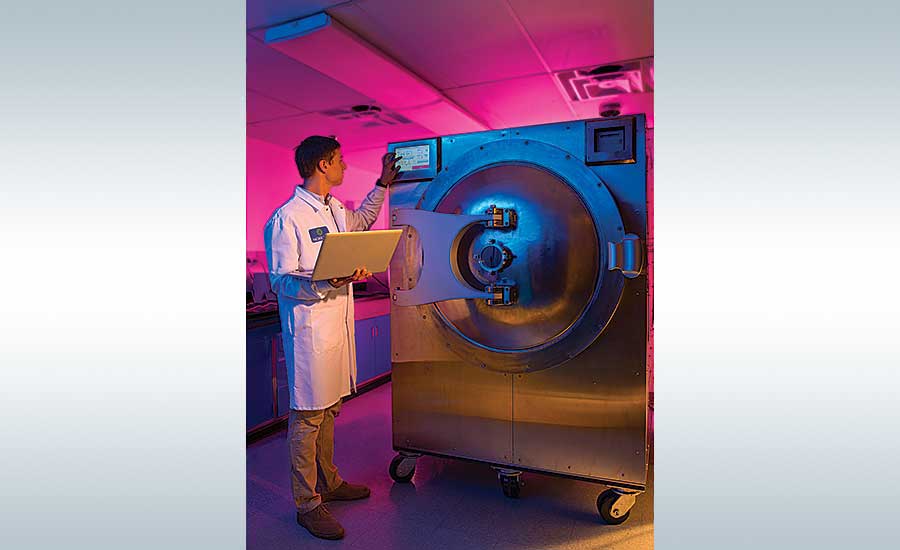
A critical advantage of NO2 sterilization is that it can be conducted at low temperatures, without a deep vacuum and in a relatively short time. Photo courtesy Noxilizer Inc.

Because EO is a gas, it cannot be used to sterilize liquids, and it cannot be used on devices that are in gas-impermeable packaging. Photo courtesy 3M Co.

A disadvantage of the EO sterilization process is time. The process can take days. Photo courtesy ETC Sterilization Systems






When it comes to sterilizing medical devices, material compatibility is the Achilles’ heel.
“Steam is probably the best sterilization method,” notes Clark Houghtling, who has worked in the sterilization industry for 40 years. But steam, technically known as moist heat, has limited use because few materials in medical devices can take the high temperature. Moist heat sterilization is often limited to products that consist of metal, glass and certain plastics that withstand high temperatures.
In contrast, ethylene oxide (EO) is the “most material-friendly sterilant,” insists Houghtling, the vice president for business development and technical affairs at the Cosmed Group, which provides contract sterilization services and supplies to medical device manufacturers. “It does not alter the physical structure of the component.”
Because it is so material-friendly, EO currently accounts for more than 50 percent of industrial product sterilization, Houghtling estimates, adding that gamma radiation is the other big player, accounting for more than one-third of the market.
Despite being material-friendly, EO does have two minor limitations, Houghtling says. Because EO is a gas, it cannot be used to sterilize liquids, and it cannot be used on devices that are in gas-impermeable packaging.
Another gas sterilant, nitrogen dioxide (NO2), is incompatible with cellulose materials, such as paper and cardboard, explains physicist David Opie, Ph.D., the senior vice president for research and development at Noxilizer Inc. NO2 also changes the chemical structure of polyurethane and nylon, as well as polyoxymethylene, which is commonly known by the brand name Delrin.
With radiation sterilization, the biggest concern is the effect on polymers, such as certain plastics like polytetrafluoroethylene, commonly known as Teflon.
“[Radiation] will create bond breakages in long-chain polymers,” says nuclear engineer Mark Smith, the managing director of the private radiation consulting company Ionaktis LLC. Caused by free radicals formed during irradiation, these breakages can make polymers more brittle, change their temperature characteristics, discolor them, and limit their shelf lives. Radiation also can change the fluid properties of plastics.
Glass will change colors when irradiated, Smith adds, noting the metal ions in glass will dictate the new color. Clear glass, for example, may turn brown. He recalls an incident in which a manufacturer used radiation to sterilize clear glass syringes but the glass turned so dark that the black gradation markings could not be read.
Material incompatibility can be addressed by adjusting the manufacturing process to accommodate the sterilization method. The syringe manufacturer that Smith noted decided to change the gradation markings to white so that they were easier to read. Medical devices sterilized with NO2 are placed in their cardboard packaging after the devices are sterilized. And when gaseous sterilants are used for devices that contain liquids, the liquids are typically sterilized in their containers by radiation prior to the containers being incorporated into the devices.
Alternatively, the sterilization method could be switched to one compatible with the materials, or the materials could be replaced with ones compatible with the chosen sterilization method. However, Houghtling points out, switching materials to address the limitations of a particular sterilization method almost always results in higher raw material costs.
“Nylon, polyurethane and Delrin—you can’t say those are uncommon materials,” Opie admits, noting that NO2 was not introduced as a sterilizing agent until approximately three years ago. “Other sterilization methods have the benefit of 30 or more years [during which] medical device engineers [have become] attuned to the incompatibilities and, just by nature, don’t select incompatible materials.... Until NO2 gets more mainstreamed and people start avoiding nylon, Delrin and polyurethane, then we’ll always be challenged with asking people to change the materials.”
Radiation physicist Chris Howard views different sterilization methods not so much as having advantages over one another but as being complementary. “There are certain products that don’t mix well with radiation, and there are certain products that don’t mix well with ethylene oxide,” says Howard, who works at Nordion Canada, which provides gamma technologies and medical isotopes to sterilization facilities in approximately 40 countries.
Sometimes, the molecular changes caused by sterilization methods are beneficial. Gamma radiation, for example, is used to harden the ultrahigh-molecular-weight polyethylene used in orthopedic implants like artificial hips and knees so that the implants will last a long time. “Those products are given healthy doses of gamma radiation several times to make them very dense so they have better wear properties,” Houghtling says.
Saving Time
The goal of all sterilants is to either kill microorganisms or make them incapable of replicating. “You can have one bad germ, but if it can’t reproduce itself, it means nothing,” Opie adds.
Typically, medical device manufacturers design their methods to achieve a sterility assurance level (SAL) of 10-6. At that level, the chances are one in a million that one microorganism remains viable, explains Smith, who has more than 30 years of experience in the field of radiation.
To reach such a SAL, different sterilization methods take different approaches.
Conventional EO sterilization, for example, historically relied on a three-phase process that begins with preconditioning. Pallets of medical devices are placed in a room, chamber or cell, where they are exposed to heat and humidity for a defined period to acclimate the devices to the sterilization conditions and to make the microorganisms more susceptible to the sterilization process.
In the second phase, the pallets are placed in a sterilizer, which can range from the size of a tabletop to a full tractor trailer. The medical devices are sterilized in their final packaging, typically corrugated cardboard boxes.
In the United States, most EO sterilizers use 100 percent EO, as opposed to a blend of EO and carbon dioxide, Houghtling notes. When 100 percent EO is used, the process is done under vacuum, creating an environment that is lower than atmospheric pressure. After air is removed from the sterilizing chamber and humidity added, EO is introduced. Several hours are required for EO to permeate throughout the load and kill microorganisms to the designated SAL. EO is then flushed out of the chamber.
For EO sterilization, it’s essential that devices are packaged in gas-permeable sterile barriers. The pores in the barriers are large enough to allow EO to flow in and out but too small to allow microorganisms in. As a consequence, once EO kills the existing microorganisms on the devices, the devices remain sterile until their gas-permeable barriers are opened.
The last phase of EO sterilization is aeration to further remove EO. This is done in a room, chamber or cell with heat, but without humidity. Aeration reduces EO concentrations to or below permissible levels for the safety of both the workers who handle the devices and the patients who are treated with them.
Coming more into vogue in EO sterilization is all-in-one processing, in which all three phases take place in the sterilizer instead of in three different areas. The all-in-one process is safer for workers because they do not move the pallets until the product is nearly fully aerated. It also reduces process deviations and product damage.
On the other hand, because the entire process is executed in a sterilizer, the amount of time that the devices are in the sterilizer roughly doubles, cutting throughput in half. So to process the same volume, all-in-one processing requires roughly doubling the number or size of the sterilizers. In addition, sterilizers are much more expensive than preconditioning and aeration areas.
However, the time required for EO sterilization can be reduced significantly by combining all-in-one processing with dynamic environmental conditioning (DEC), parametric release and in-chamber aeration, Houghtling notes.
DEC, which works best for products that can withstand deep vacuums, can be used to more quickly and evenly heat and humidify product loads. Parametric release eliminates the need for using biological indicators to monitor whether the designated SAL was reached, which typically takes two to seven days. In addition, the dynamics of the sterilization chamber can be used to speed up aeration, resulting in more rapid dissipation of residual EO.
“It can take a process that may occupy five to 10 days and shorten it to perhaps one day,” Houghtling reports. “This is arguably the biggest advance in the EO sterilization process since its beginning in the 1950s.”
The phases of NO2 sterilization mimic those of EO, with a major difference being that medical devices are not sterilized in their cardboard packaging. Consequently, NO2 sterilization is more likely to be done in house than outsourced.
Opie notes that two-door sterilizers can be used to batch-sterilize medical devices in line. The devices are manufactured and packaged in sterile barriers in a clean room, moved into an NO2 sterilizer through its loading door in the clean room, sterilized, and removed through the opposite door into a normal manufacturing area to be packaged and labeled.
“You want the size of the sterilizer to match the speed of the packaging line,” Opie says. “If you have a two-hour cycle for sterilization, for example, then you need two hours’ worth of product to fit in the chamber.”
Sterilizing With Radiation
While EO and NO2 sterilization takes place in sealed chambers, radiation sterilization typically takes place within a concrete shield approximately 2 meters thick. Packaged medical devices travel through an entrance in the shield on a conveyor that takes a series of turns before reaching the radiation source in the inner chamber of an irradiator, Smith explains. Radiation does not escape from the shielded area because it is absorbed by the concrete walls.
The most common source of radiation for sterilization is cobalt-60. Small rods of cobalt-60 are stacked in a column that is encapsulated by two separate layers of stainless steel. Each “pencil” of cobalt-60 is approximately 18 inches long and 0.375 inch in diameter.
Several pencils are placed in the source rack of an irradiator. As the cobalt-60 decays, more pencils are added to maintain the irradiator’s strength. Eventually, pencils are replaced either because they have decayed too much to be useful or because the source rack no longer has room for fresh pencils.
Cobalt-60 emits gamma rays at a steady rate in all directions as it decays. Consequently, products like packaged medical devices are circulated around the source rack. The gamma rays penetrate the products and damage the DNA and other cellular structures of microorganisms.
Other forms of radiation used to sterilize medical devices include electron beam (e-beam) and X-ray. Both are generated by accelerators, not radioactive sources. An X-ray irradiator is essentially an e-beam irradiator in which electrons pass through a target that converts the electrons to X-rays. X-ray’s ability to penetrate products is comparable to gamma, while e-beam penetrates only a few centimeters.
Unlike gamma, both e-beam and X-ray are directional. “If you want to irradiate a product with electron beam or X-ray, your beam is pointing straight at it,” Smith says. Consequently, products can be sterilized one box at a time with e-beam and one container at a time with X-ray.
E-beam and X-ray deliver energy at a higher dose rate than does gamma. This allows free radicals to form and recombine more quickly, reducing degradation in such materials as oxygen-permeable polymers.
“At a slower rate, there’s more time for the oxygen to permeate through a polymer...which then creates the oxygenation reaction and creates more degradation,” Smith explains. “With electron beam in particular, you’re doing that fast enough that the oxygen doesn’t have [as much] time to go in and react to those free radicals.”
Other Pros and Cons
One major advantage radiation has over gaseous sterilants is speed. Large radiation facilities can typically sterilize products in one to two hours.
“[EO facilities] have to allow for the gas to dissipate after the product has been exposed to it. That can take days in some cases,” adds Terry Kehoe, Nordion’s senior account manager.
In contrast, irradiated products are safe to use as soon as they come out of an irradiator.
With radiation sterilization, sterile barriers do not need to be gas-permeable. Foil packaging can be used instead, which is especially critical for medical products that should not be exposed to relative humidity, such as bioabsorbable products.
For better and worse, gamma radiation cannot be turned off, unlike e-beam and X-ray. For safety, radioactive pencils are transported in heavily shielded shipping containers. And any time a gamma irradiator is not being used, the cobalt source rack is lowered into a pool of water to contain the gamma rays.
On the other hand, because cobalt-60 is not dependent on an outside power source, it is reliable, simple, and easy to control, Howard says. It also produces very repeatable results.
Another advantage is that gamma irradiators require relatively few spare parts. “Cobalt is a fairly simple design. You’ve got a conveyor. You’ve got something that moves the sources up and down. That’s pretty much it,” Smith says. “For e-beam and for X-ray, you’ve got a whole particle-accelerator system…so there are a lot more spare parts.”
Unlike gamma irradiators, e-beam and X-ray accelerators require an “astronomical” amount of electricity, Smith says. As a result, accelerators produce a great deal of heat and must be water-cooled.
While EO is more material friendly than other sterilants, it is flammable and explosive. EO sterilizers must be located in areas built with damage-limiting construction and intrinsically safe electrical fixtures.
In addition, EO is harmful to people at low doses, and it is labeled carcinogenic, notes Noxilizer’s Opie. In contrast, NO2 is harmful to people at high doses, so it is easier to reduce NO2 concentrations on medical devices to safe levels during aeration than to reduce EO concentrations.
“All the regulatory agencies around the world are putting much more strict limitations on human exposure to stray ethylene oxide,” Opie says. “You have to have a full respirator on to handle those products in a lot of places right now.”
A critical advantage of NO2 over EO is that NO2 sterilization can be conducted at low temperatures, without a deep vacuum and in a relatively short time. As a consequence, NO2 can sterilize the exterior surfaces of syringes and other drug-delivery systems with minimal to no effect on the medicine in those systems.
Elastomeric closures, such as pistons in syringes and stoppers in vials, are vulnerable points in drug-delivery systems. “EO goes right through those elastomeric closures and contaminates the contents,” Opie says.
Ultimately, the best sterilization method is the one that works best for each particular product. “All sterilization methods have value when they work effectively and efficiently,” Houghtling says. “Several key factors, such as material compatibility, cost and turnaround time, need to be analyzed, and then the optimum method can be selected.”
Looking for a reprint of this article?
From high-res PDFs to custom plaques, order your copy today!